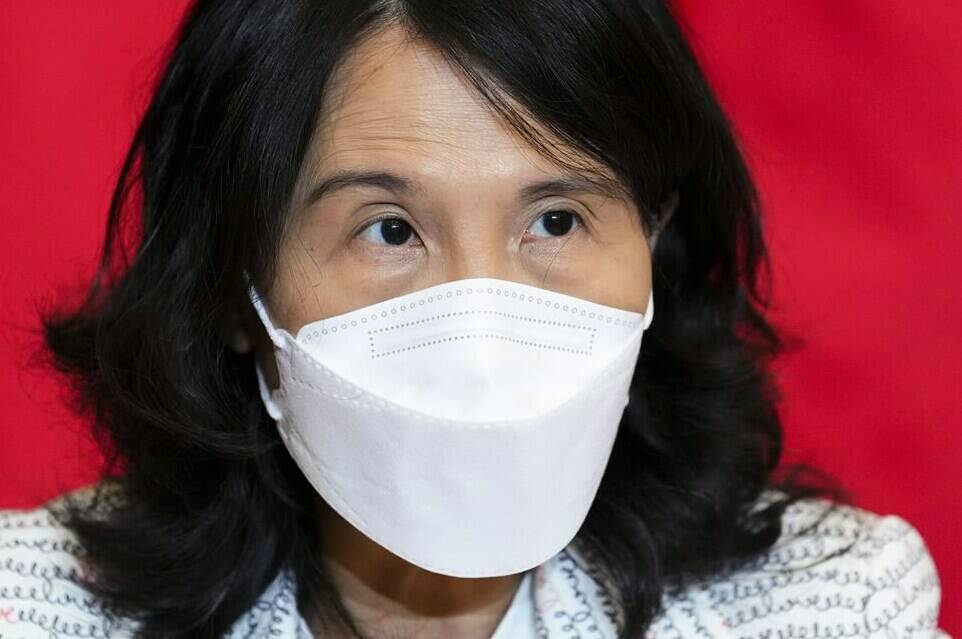
Canada’s chief public health officer says COVID-19 is still circulating at a “relatively high level” and other strains of influenza may surge in the new year.
At the same time, governments need to invest in preparing for and preventing future epidemics, Dr. Theresa Tam says.
In a year-end interview with The Canadian Press, Tam urged Canadians to “remain vigilant” and said what happens next with COVID-19 and flu depends largely on people taking precautions for the holidays – including staying up to date with vaccinations, masking indoors in crowded conditions or when seeing vulnerable family members and staying home when not feeling well.
“I always say that, you know, we own the situation,” she said. “We can make the decision and influence the trajectory of the pandemic curve… We know what we could do to reduce our risks, particularly when the hospitals are so pressured.”
Tam said it’s also important to remember that the antiviral drug Paxlovid is available for people who do get sick to decrease their risk of severe illness and hospitalization.
“I would advise people, especially (those) at high risk, to think ahead,” she said.
“Plan ahead with your health professionals, know where you can access Paxlovid and know how you can get your rapid test or get testing done if you should get sick. That will ensure that you can get access to the drug as fast as possible.”
The virus that causes COVID-19 continues to evolve, Tam said, and she’s eyeing a surge of COVID-19 cases during Australia’s summer right now to try to predict what it might do in this hemisphere. It’s too early to say whether further booster shots might be necessary, she said, but Canadian health experts will “regroup in the new year” with other experts internationally to come up with further guidance.
“The general good news is that even when cases surge, ICU admissions and deaths are relatively low, so this is what we need to track — because right now our overall goal is to reduce serious outcomes,” she said.
As for influenza, the H3N2 strain that has sent many children and seniors to hospital “spiked very fast and early,” and it’s possible that it could come down quickly, Tam said.
But she’s watching to see if the other Influenza A strain — H1N1 — emerges, as well as Influenza B, which could come later in the flu season and “affect children in particular.”
As we manage these diseases, Tam said we need to improve our readiness for more epidemics to come.
“(The COVID-19 pandemic) is one of the most teachable moments, I think, in our collective lifetimes,” she said.
Although Canada and other countries may have been good at “ratcheting up response” to the crisis, it’s become clear that “prevention and preparedness” needs more attention.
“There’s much more investment when… the house is on fire and putting out the fire than there is to build the fire stations and get prepared and get rehearsed ahead of time, even for a rare event,” Tam said.
Factors like climate change, which affects the way animals and humans interact, can lead to more disease transmission and epidemics “might not be so rare,” she said.
“We need to be prepared,” Tam said. “I’m not talking about just Canada, (I’m talking) globally.”
That preparedness includes a global approach to health and “better data and surveillance systems to monitor viruses and other harms that could impact both human… and animal health and the environment.
“And that gives you an earlier signal, perhaps, to reduce and mitigate viruses or other pathogens that can affect humans.”
Another element of future disease prevention is to pay more attention to “the hidden pandemic” of antimicrobial resistance, Tam said.
The World Health Organization has identified antimicrobial resistance, which happens when bacteria and viruses no longer respond to antibiotic and antiviral medications, as a major threat to human health.
“If antibiotics don’t work, we are in a situation a bit like (we were) the beginning of this pandemic, where we have no effective countermeasures,” Tam said.
These kinds of threats were difficult to explain to decision-makers before COVID-19 struck, she said.
Public health has been “underappreciated and I think underinvested,” Tam said.
But now that governments have been involved in responding to a pandemic, “they understand a bit more about what public health does and the importance of public health.”
A big part of public health’s role, Tam said, is to “highlight health inequities” among vulnerable populations.
COVID-19 has shown that in addition to people who are elderly and those with underlying health conditions, those struggling with poverty, people who are homeless, racialized groups, Indigenous people and people suffering from addiction are “severely impacted” during crises, she said.
“Thinking about preparedness in a different way in reducing health inequities will get us (into) a better place for the next pandemic,” Tam said.
—Nicole Ireland, The Canadian Press
RELATED: Officials eyeing COVID-19 variant evolution as early signs point to fall resurgence
RELATED: Federal government to end COVID-19 vaccine mandates: sources