A Vancouver pilot program shows take-home fentanyl tests can encourage some people to use less and use in a safer setting.
The results were released this month in the International Journal of Drug Policy, but the program itself ran back in the spring of 2019.
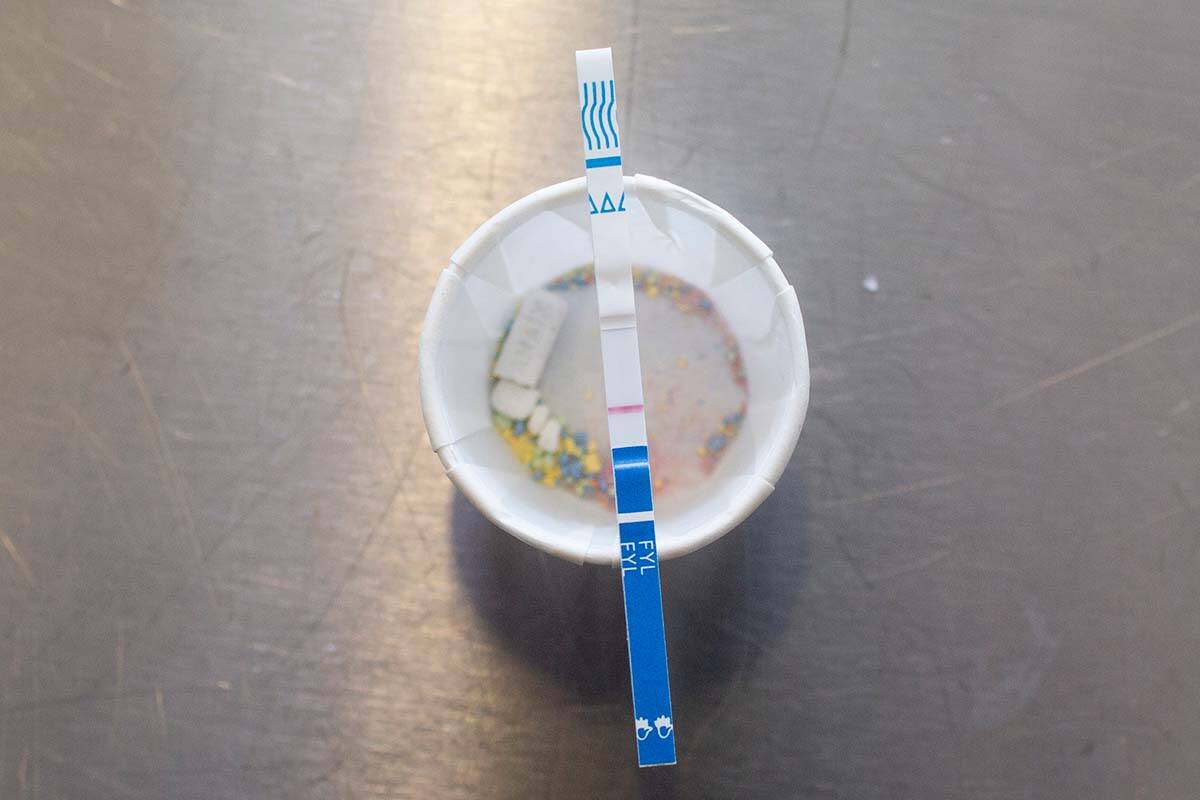
A collaboration between Vancouver Coastal, Interior and First Nations health authorities, the BC Centre on Substance Use (BCCSU) and the BC Centre for Disease Control (BCCDC), the program distributed 1,680 take-home tests to 218 participants from 10 drug-checking services in Metro Vancouver.
Participants were provided with clear instructions on how to use the tests and were asked to report any behavioural changes if they did find fentanyl in their drugs. In 27 per cent of those instances, researchers say participants made at least one safer choice. Those included taking less of the drug, not using it at all, choosing to take it with someone else present or at a safe consumption site, or asking someone to check in on them.
“These findings demonstrate that in the absence of a regulated drug supply, strategies that provide people with information about the substances they’re consuming are paramount to keeping them safe,” lead author and associate director with the BCCSU clinical addiction medicine fellowship program, Dr. Sukhpreet Klaire, said in a news release.
Findings from the BC Coroners Service show the vast majority of fatal drug overdoses occur in a place of residence, whether it’s someone’s home, a shelter or social housing site, or a hotel. In the first three months of 2022, 548 people died of toxic drug overdoses, 80.5 per cent of which occurred in a residence.
The take-home fentanyl tests look to target this trend, according to the researchers. They also hope to expand the safety of supervised consumption sites, where no deaths have occurred in B.C. to date, according to the BC Coroners Service.
To test the effectiveness of the take-home tests, the researchers compared their fentanyl-positivity rates to those of samples tested at drug-checking sites during the same period. They found the tests’ rates almost exactly aligned, at 89.1 per cent for take-home ones and 90 per cent for on-site ones.
The researchers did note two drawbacks to the take-home tests, however: they didn’t accurately test for stimulants, and could only test for the existence of fentanyl not the quantity.
Still, the researchers considered the program a success. Of those who participated, 96 per cent said the test instructions were easy to follow and 95 per cent said they would use them again.
Since the pilot was first conducted, Vancouver Coastal Health has expanded the number of sites providing take-home tests from 10 to 20, and Interior Health, Island Health and Fraser Health have each introduced sites of their own.
The researchers say more work needs to be done to determine how and if use of the tests actually reduces the number of overdoses, but that at the very least they provide people who use drugs with potentially life-saving information and greater agency.
READ ALSO: ‘Death penalty situation’: 6 years ago, B.C. declared toxic drug poisonings a health emergency
READ ALSO: Safe-supply pilot project findings promising, but advocates say more action is needed
@janeskrypnek
jane.skrypnek@bpdigital.ca
Like us on Facebook and follow us on Twitter.