An alternative mental health court program designed to fast-track people with untreated schizophrenia and other psychotic disorders into housing and medical care — potentially without their consent — kicked off in seven California counties, including San Francisco, on Monday.
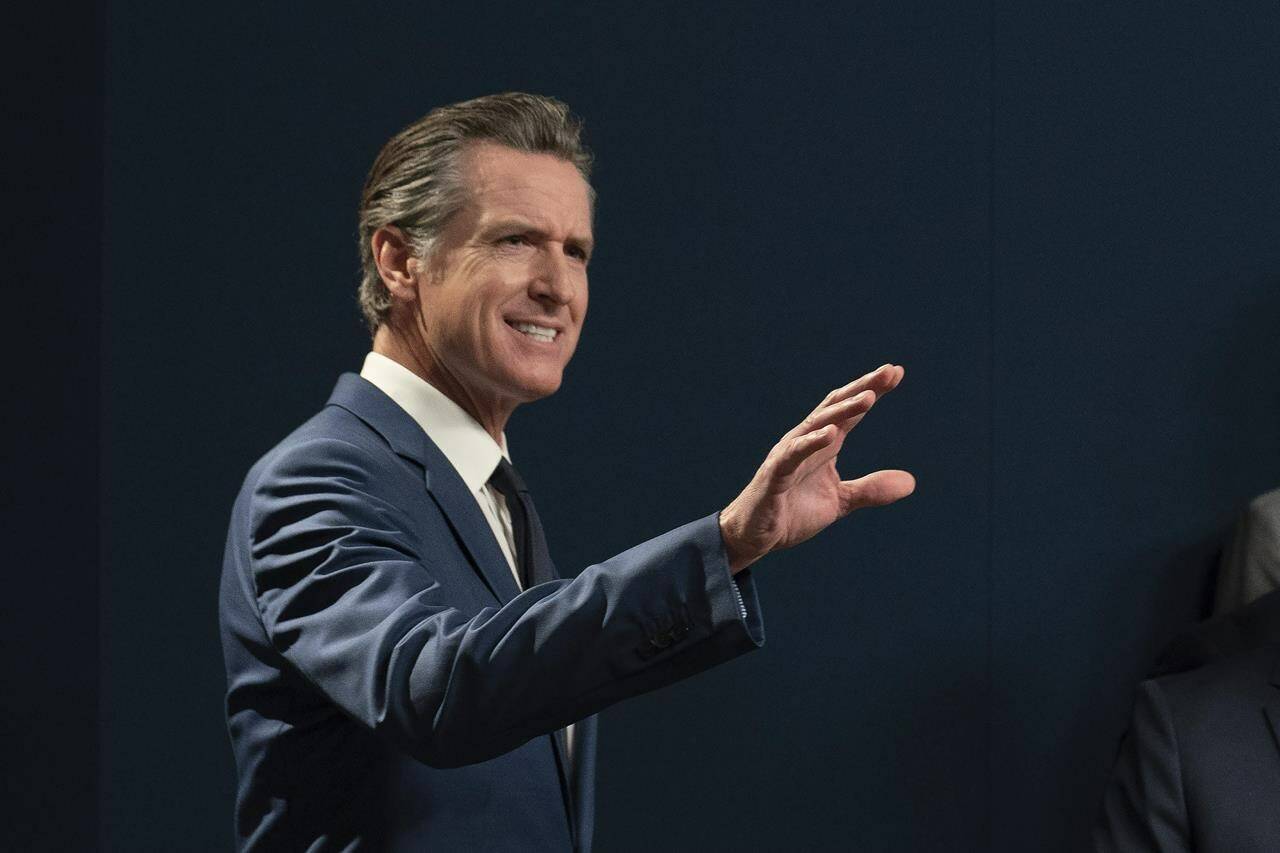
Democratic Gov. Gavin Newsom created the new civil court process, called “CARE Court,” as part of a massive push to address the homelessness crisis in California. Lawmakers approved it despite deep misgivings over insufficient housing and services, saying they needed to try something new to help those suffering in public from apparent psychotic breaks.
Families of people diagnosed with severe mental illness rejoiced because the new law allows them to petition the court for treatment for their loved ones. Residents dismayed by the estimated 171,000 homeless people in California cheered at the possibility of getting them help and off the streets.
Critics blasted the new program as ineffective and punitive given that it could coerce people into treatment.
But as petitions roll in Monday, it’s not clear who the program might help nor how effective it will be. That’s because the eligibility criteria is narrow and limited largely to people with untreated schizophrenia and related disorders. Severe depression, bipolar disorder and addiction by itself do not qualify.
“It’s hopefully going to help some people who need some help, and it is probably not going to make a huge dent in what you observe in the community,” said San Francisco Superior Court Judge Michael Begert, who will supervise the court.
Here are things to know about the new system:
WHAT IS “CARE” COURT AND WHO IS ELIGIBLE?
Dr. Mark Ghaly, secretary of the California Health and Human Services Agency, said in a news briefing last week that the program is aimed at catching people before their condition worsens.
Family members and first responders are among those who can now file a petition on behalf of an adult they believe “is unlikely to survive safely” without supervision and whose condition is rapidly deteriorating. They also can file if an adult needs services and support to prevent relapse or deterioration that would likely result in “grave disability or serious harm” to themselves or others.
To be eligible, the person needs a diagnosis on the schizophrenia spectrum or other qualifying disorders. People with severe depression or bipolar disorder do not qualify. A person does not have to be homeless to be eligible.
A special civil court in each county will review each petition with the county behavioral health agency evaluating eligibility. The individual will be appointed a lawyer and a support person of their choice.
If the court determines the individual meets eligibility criteria, they will be asked to work with the county on a voluntary plan that includes housing, medication, counseling and other social services. The agreement would be in effect for up to a year with the possibility of extending it for another year.
If all parties cannot agree to a voluntary plan, the statute says the court will order they work on a plan.
WHAT HAPPENS IF THE PERS
ON DOES NOT WANT TO PARTICIPATE?
Civil rights advocates have raised fears that the new process will result in vulnerable people being forced into treatment.
A person who does not successfully complete a plan could be subject to conservatorship and involuntary treatment, said Tal Klement, a deputy public defender in San Francisco who is among critics of the new process.
But the statute also allows the court to dismiss the proceedings if the individual declines to participate or to follow the agreement. Judge Begert, in San Francisco, said he cannot compel someone to engage; the best he can do is start building a relationship with the person.
Veronica Kelley, Orange County behavioral health director, said the county’s judges understand building rapport with eligible candidates takes time and have agreed to grant her team extra time to reach voluntary agreements, despite the statute’s deadlines.
ARE THERE ENOUGH HOMES, TREATMENT BEDS AND SUPPORT?
The state has allocated money for emergency shelters but critics say there is a constant shortage of case managers, appropriate in-patient treatment facilities and supportive housing.
San Francisco officials said in a statement that about 10% of more than 2,500 beds are open for new people. The treatment beds range from detox to step-down care for people leaving long-term care.
Opponents of the program say the state should have invested in more housing and existing services rather than establishing a new court system.
“The issue is not that these resources are available and people aren’t using them,” said Samuel Jain, senior policy attorney at Disability Rights California. “It’s that these voluntary community-based services are under-resourced and not accessible.”
WHAT HAPPENS IF THE PERSON IS NOT ELIGIBLE FOR CARE?
The National Alliance on Mental Illness in California, a grassroots organization supporting people with a mental illness and their families, pushed for the new mental health program. Some family members have long wanted a way to order their loved ones into treatment, the organization said.
Jessica Cruz, the group’s CEO, encourages people not to give up if their family member does not qualify because other resources may be available.
“For us, it is just really about making sure that our loved ones have the best life that they could possibly have,” she said. “Living on the streets and dying on the streets is not the way for anybody to live.”
WHICH COUNTIES ARE ACCEPTING PETITIONS?
San Francisco, Orange, San Diego, Riverside, Stanislaus, Tuolumne and Glenn counties launched the new program Monday. Los Angeles County will begin its program Dec. 1.
The state estimates roughly 1,800 to 3,100 people could be eligible in the first seven counties. Los Angeles could bump up estimates to 3,600 to 6,200, although uptake could take time.
The rest of the state has until December 2024 to establish mental health courts.