People who use drugs are facing barriers to treatment when seeking recovery – many have been around for years while others cropped up during COVID-19.
With over 2,272 suspected illicit drug toxicity deaths in British Columbia, 2022 had the second-highest illicit drug death rate ever recorded, according to the BC Coroners Service.
The supply of illicit drugs is growing increasingly toxic as they are mixed with such compounds as fentanyl and etizolam – the latter of which is not responsive to naloxone, the medication used to block the effects of opiods.
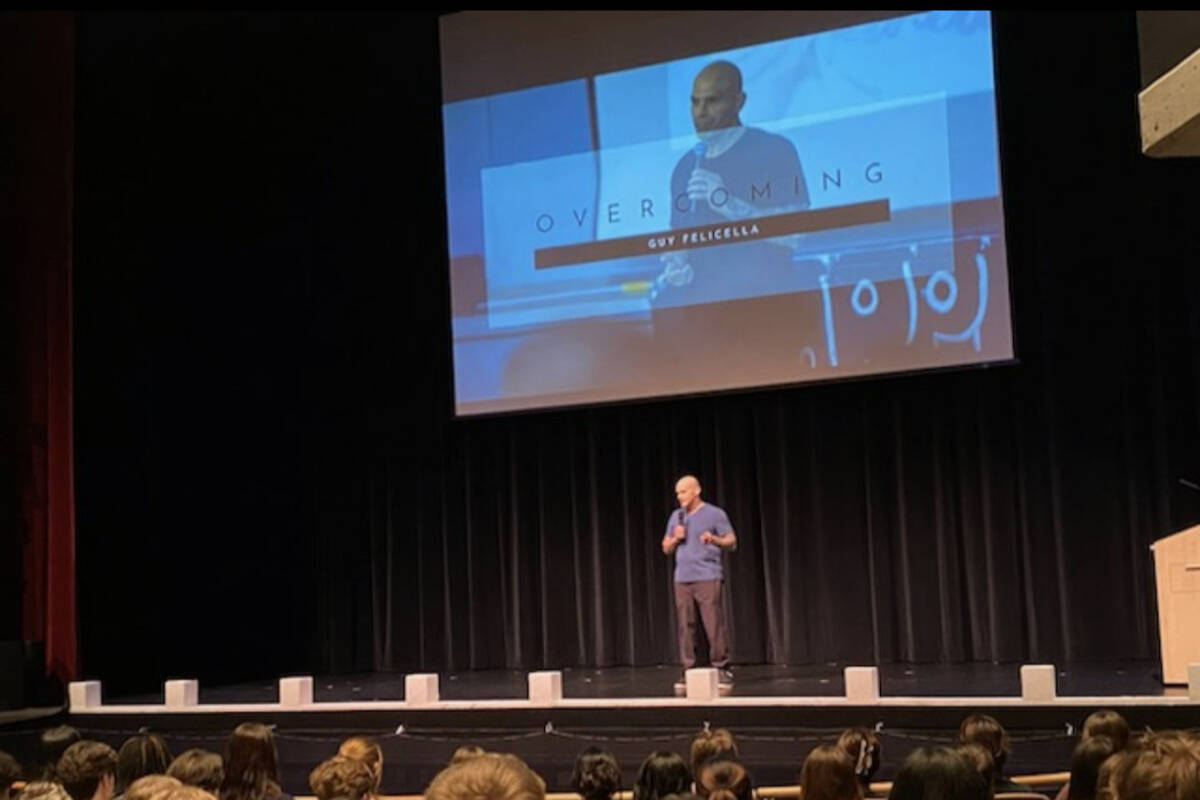
These dangerous compounds lurking in an unchecked supply are only exacerbating the need for more harm reduction and better access to addiction care, says Guy Felicella, a Vancouver-based advocate who credits harm reduction like drug checking and safe-use spaces for saving his life.
The system, he said, isn’t keeping up with the toxic drug supply.
“We just need to give people the opportunity so that when they are ready, we are ready,” he said. “That is the quintessential factor in people moving forward.”
The things he said British Columbia needs more of – and less of – could save countless lives, giving people who are addicted to drugs a chance at a life that isn’t centered around using. Such problems as long waitlists, doctor shortages, medication stigma and payment processes, however, are holding people down, Felicella said.
READ MORE: Chief coroner prescribes ‘urgency’ as B.C. records 2,272 toxic drug deaths in 2022
Felicella said getting on a waitlist for a detox centre is the first challenge people face.
In Victoria, that looks like going to Central Access and Rapid Engagement Services (CARES) for a referral. The front desk at CARES said the time it takes to move through that step depends on the circumstances, but can sometimes take a few days.
Fred Cameron, who works for SOLID Outreach Society, a non-profit organization which provides support services and harm reduction, said the referral process can be bumpy.
“The process to get into detox is not as smooth as it could be,” Cameron said. “The referral process is not open to the public – you can’t just do it online. Small NGOs (non-government organizations) aren’t able to do that either, so there are definitely some hoops you have to jump through to get there.”
After the referral is sent to Island Health, patients go on a waitlist for a detox bed, which can take weeks, but more commonly, months. There are 3,201 publicly funded community substance-use beds in the province and research shows there is an estimated 83,000 British Columbians with an opioid addiction alone, according to Kevin Hollett at the BC Centre on Substance Use (BCCSU).
Hollett said the number could be higher, since many addictions are undiagnosed. Not everyone with an addiction needs to detox, and there are private facilities available, but they can be expensive. The government-funded bed-to-person ratio in B.C. is one of the barriers Felicella cites.
Abstinence-only programs that limit and stigmatize certain medications also pose problems, Felicella said, adding that some publicly funded treatment centres still don’t allow the use of methadone, a medication used in Opioid Agonist Therapy (OAT) to treat withdrawal symptoms, which Felicella said can last for months and decrease the likelihood of stabilization and ability to learn life and coping skills.
Additionally, research from BCCSU shows patients are at a higher likelihood for overdose if they discontinue the use of methadone for OAT.
Cheryl Diebel, the director of New Roads Recovery Centre in Victoria, said there are facilities that don’t allow methadone use during OAT, but many are moving away from this.
“That’s a very, very purist view of abstinence – we absolutely allow OAT and we recommend that patients don’t do any kind of withdrawing from the methadone for at least the first two months so we know they are starting to stabilize,” she said.
Evan James, who works with the Umbrella Society, an organization in Victoria that provides addiction support, said income assistance requirements are one of the more frustrating barriers he sees every day. For publicly funded treatment centres, he said patients either need to be on income assistance or disability, but many don’t qualify for either.
“We have this huge slice of the population in between the two – they certainly cannot afford the expensive private paid treatments, but they are not eligible for income assistance because they haven’t lost everything, or they have assets, or they’re still working – whatever the case may be,” James said.
READ ALSO: Falcon promises $1.5 billion ‘no-cost recovery-oriented’ approach toward addiction
James said cost barriers, coupled with the fact that most patients need to go to the mainland for publicly-funded treatment, present challenges to recovery. Support systems during recovery are essential, James said, so when people leave Victoria to get treatment, they lose that. Then the support systems they build on the mainland during treatment are lost when they come home.
Accessing alternatives to detox and inpatient treatement such as group meetings is also limited, as Cameron said the recovery world fell apart when COVID-19 first hit.
“A lot of the events and public gatherings that took place outside of structured recovery groups were cancelled and put on hold, so a lot of the things that I look back to that helped me out currently don’t exist,” he said. “There is a place for professional recovery, but to imagine a system that is big enough and comprehensive enough to help everyone – I just can’t see it, which is why people are directed to 12-step programs. It is those kinds of groups that people are going to and getting support in the early days.”
For a system to be successful in helping people recover, advocates say more of everything is needed.
Diebel said more beds, specifically women’s beds, are needed. Cameron said more harm reduction services and different outlooks on recovery would help. James said addiction treatment needs to be treated as a medical expense by the province and Felicella said in general, the process needs to be easier to navigate.
“There are people who want help,” Felicella said. “Society often says ‘these people don’t want help, they’re not going to change,’ but they’re not changing because it’s hard to get access to change. Instead of pointing fingers and blaming people struggling with addiction, let’s start pointing fingers at the policies that hinder them from getting the help that they need.”
@HLFerguson
hollie.ferguson@vicnews.com
Like us on Facebook and follow us on Twitter.
addictionsAddictions treatment